Probiotics, Prebiotics, and Beyond! Treatment and Prevention of Antibiotic-Associated Illnesses
Antibiotics have been life-saving miracle drugs of the 20th century. However, the problem of antibiotic-resistant superbugs and microbiome disruption has posed a serious health threat in the 21st century. The average Canadian takes one course of antibiotics every 18 months. Unless specific action to reestablish microbiome balance is taken, antibiotic use poses a two-part health risk by:
- Creating antibiotic resistance
- Increasing antibiotic associated illnesses
Antibiotic resistance is the increased spread of disease-causing bacteria “superbugs” that are resistant to antibiotic treatment. It is estimated that by 2050, 2.4 million deaths in developed countries (Canada, USA, Australia, New Zealand) will be due to untreatable antibiotic-resistant infections.[1]
Antibiotic-associated illnesses are conditions caused by microbiome disruption. Statistics show that increased antibiotic use is directly related to an increase of the following diseases:[2]
- Allergies
- Eczema
- Intestinal diseases (SIBO, Candida overgrowth, IBS)
- Autoimmune conditions
- Metabolic diseases (diabetes, metabolic syndrome, childhood obesity)
With the increase of antibiotic overuse in farming, medicine, and hospital care, it has become essential to treat with probiotics to rebalance the microbiome whenever antibiotics have been used in patient care.
What’s the Microbiome?
Picture a rainforest—an ecosystem of diverse and undiscovered species living in a delicate balance, the product of millennia of evolution. The human microbiome is similar to a rainforest with diverse microorganisms living in balance (bacteria, fungi, parasites, and viruses). These microscopic inhabitants live inside and on the surface of our bodies and have evolved with humans over time. The human body is made up of 40 trillion cells, of which 30 trillion are the microbiome. In other words, ¾ of our cells live in the microbiome, making us proportionately more microorganisms than human!
Probiotics are sources of the beneficial or “good” bacteria that live inside our bodies and make up a large part of our microbiome. Fermented foods have been the main source of probiotics for centuries. For therapeutic use, concentrated isolated probiotic strains are available as supplements.
In clinical practice, the two most common questions patients ask about probiotics are:
- Why do I need to take probiotics?
- How long do I need to keep taking this for?
After considering your health history since birth, the answer is two-part:
- What is your current diagnosis and symptoms?
- What is the state of your microbiome? Your microbiome can be evaluated with specific lab tests which assess the health of your microbiome—ask your health-care provider for details.
 What does the microbiome do? The microbiome maintains and manages several essential functions in the body:
What does the microbiome do? The microbiome maintains and manages several essential functions in the body:
- Balances the immune system throughout life (from birth till end of life)
- Supports essential metabolic functions:
- Regulates gut-brain axis (neurotransmitters serotonin and dopamine produced in the gut, travel to the brain, and regulate mood)
- Mitochondrial function (energy production inside every cell in the body, except red blood cells)
- Detoxification
- Food supply for good bacteria and intestinal cells (short-chain fatty acids)
- Antiinflammatory (inflammation is part of every illness; it prolongs and complicates recovery from illness, interferes with healing, and is the source of physical pain)
Antibiotics are the main disruptor of microbiome balance and function. As a result, antibiotic-associated illnesses such as allergies, eczema, autoimmune conditions, childhood obesity, as well as intestinal and metabolic diseases, are on the rise.[2]
Treatment and Prevention of Antibiotic-Associated Illnesses:
Prebiotics are the good food which feed your good bacteria. Soluble fibre is a prebiotic which comes mainly from plant-based foods. The SAD (standard american diet) has about 4 g of soluble fibre present, whereas the Mediterranean diet has about 15–20 g of soluble fibre. Canada’s updated Food Guide emphazises plant-based nutrition, which is a great source of prebiotic fibre.
- Food sources of prebiotics: beans, root vegetables, apples, pears, broccoli, and Brussel’s sprouts are some good sources of soluble fibre.[3]
- Probiotic foods: all the fermented foods (usually lactofermentation) such as sauerkraut, and pickled vegetables such as carrots, beans, beet, onions, garlic, kim-chi, and olives.
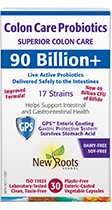
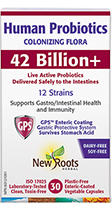
- Probiotic suppplements: Is my probiotic strong enough? For small intestine conditions such as IBS and small intestinal bacterial overgrowth (SIBO), a minimum of 10 billion Lactobacilli and Bifidobacteria cells has been shown to be clinically beneficial. For large intestine conditions such as Crohn’s and ulcerative colitis, a minimum of 50 billion Lactobacilli and Bifidobacteria cells is often recommended by clinicans and supported with research.
It is important to work with a qualified and trained clinician, such as a naturopathic doctor, when starting and monitoring any treatment plan.
References
- OECD. Stemming the Superbug Tide: Just A Few Dollars More. · https://www.oecd.org/health/stemming-the-superbug-tide-9789264307599-en.htm · Published 2018-11-07.
- Plummer, Nigel. Antibiotics and Probiotics, Potent Manipulators of the Microbiome. Webinar.
- Health Canada. Canada Food Guide. · https://www.canada.ca/en/health-canada/services/canada-food-guide/resources/resources-download.html · Modified 2019-06-24.

 Stores
Stores