Starting Young: Sustaining Bone Health as We Age
Most of us are aware of the changes our body will undergo as we age but often think that since this is a normal process, there is nothing we can do to prevent age-related complications that may arise. With a little bit of understanding and some proactive diet, lifestyle, and supplement changes, we can absolutely protect our bones and maintain the youth of our skeletal systems.
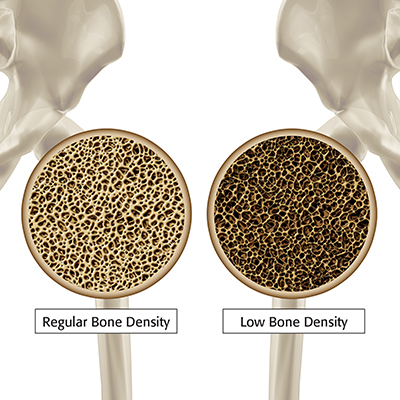
As we age, we see a reduction in the density of our bones, meaning they become brittle and at an increased risk of fractures or breaks.[1]
This is especially true in postmenopausal women due to a drop in the hormone estrogen, which leads to the body breaking down the bones faster than it repairs them.[2] We also see less fluid in our joints, which makes cartilage (the protective layer at the ends of our bones) rub together and ultimately break down, which puts the bones at greater risk of experiencing damage and pain.[3]
Finally, we see a major reduction in muscle mass as we age, usually because of a less active lifestyle.[4] With muscle, if you don’t use it, you will lose it! As muscle mass decreases, joints are less flexible, and this combination leads to an increased risk of falls, which of course increases our risk of injuries and broken bones.[5]
Osteoporosis and Osteoarthritis
These changes lead to two common yet preventable age-related conditions: osteoporosis and osteoarthritis.
Osteoporosis is low bone mineral density which is caused from a breakdown in the microstructure of the bone and leads to a predisposition to bone fractures.[6]
In one study, it was found that over 50% of postmenopausal women will have some sort of osteoporotic fracture at some point.[7] While men have a slightly smaller fracture risk (20%), they have significantly worse long-term outcomes while healing from these fractures.[8] This means the most effective way to treat these fractures—and potentially improve quality of life—is to prevent them from happening by maintaining appropriate bone mineral density.
Osteoarthritis occurs when cartilage in a joint breaks down, resulting in changes to the structures of the underlying bone.[9]
It is very common, with 80% of the US population being impacted by the condition.[10] Osteoarthritis will typically present as joint pain, stiffness, and reduced function in the affected joint, and is often caused by overuse or injury.[11]
Preventing Onset
The good news is that, while these conditions can be debilitating when severe, there are ways to prevent the onset of the condition. The most important focus should be diet and lifestyle. When you are exercising, it is important to choose weight-bearing or resistance exercise, as this has been proven to build and maintain both bone and muscle mass.[12] It is also important that any injuries are rehabilitated properly so you are not jumping back into an exercise program that could result in more damage to an injured joint.[13]
 Diet
Diet
It is essential that you choose calcium- and vitamin D–rich foods, as these minerals are important for building and maintaining the integrity of your bones.[14] These nutrients—along with other bone-supporting nutrients—can be found in dairy products, fish (especially with bones), legumes, nuts, and seeds.[15] When considering a bone-healthy diet, it is important to reduce sugar, especially while healing a joint injury.[16] Sugar has been shown to lead to more inflammation, which can in turn lead to an increase in the incidence and severity of osteoarthritis.[17]
Stack the Odds in Your Favour
Some supplements have been proven effective for maintaining bone health, especially because it can be hard to get enough calcium and vitamin D from diet alone.[18] Food is always the best source of a nutrient, but when you cannot meet your requirements, the best supplement is one that mimics the naturally occurring form of the nutrient.
In the case of calcium, this means looking for calcium hydroxyapatite, which has been shown to outperform the calcium carbonate that is typically found in supplements, both for reduction of bone loss and for having less side effects.[19], [20]
Vitamin D levels tend to drop as we age, but studies have shown that supplementing vitamin D may reduce fracture risk through its impacts on muscle function, reducing inflammation, and improving bone mineralization.[21]
Vitamin K is another important nutrient that supports calcium metabolism and ensures calcium is deposited into the bones.[22] Low levels are associated with increased fracture risk.[23]
 While calcium is key for maintaining bone health, it is important to remember that it should always be combined with other nutrients, especially vitamins D and K.[24] High doses of calcium on their own have been shown to increase the risk of cardiovascular events;[25] this can be easily prevented by choosing a multinutrient supplement rather than having calcium on its own.
While calcium is key for maintaining bone health, it is important to remember that it should always be combined with other nutrients, especially vitamins D and K.[24] High doses of calcium on their own have been shown to increase the risk of cardiovascular events;[25] this can be easily prevented by choosing a multinutrient supplement rather than having calcium on its own.
Glucosamine and chondroitin have been shown to prevent joint-space narrowing in osteoarthritis in more than one meta‑analysis.[26], [27], [28] It is important to keep in mind that this structural benefit takes 1–2 years to be achieved.[29]
Glucosamine and chondroitin are more effective when taken in earlier years, rather than being started after the onset of osteoarthritis-related pain and stiffness.[30] Chondroitin and glucosamine are key molecules in the collagen network of joints, and they help the network to sustain pressure and weight.[31] In osteoarthritis, this network is damaged and unable to bear weight as it once did, so by preventively taking glucosamine and chondroitin, we should see a reduction in the breakdown of this collagen network.[32]
Whether you are in your early 20s or heading towards retirement, it is never too late—or too early—to start supporting your bone health so that you can enjoy a youthful skeleton for many years to come.
 Dr. Kaitlyn Richardson, ND, HbSc
Dr. Kaitlyn Richardson, ND, HbSc
A naturopathic doctor in Milton, Ontario, with a clinical focus in sports and performance medicine, she believes in using individualized, holistic, and evidence-based strategies to help active individuals feel and perform their best.
drkaitlynrichardson.com
References
[1] Padilla Colón, C.J., I.L. Molina-Vicenty, M. Frontera-Rodríguez, A. García-Ferré, B. Ponce Rivera, G. Cintrón-Vélez, and S. Frontera-Rodríguez. “Muscle and bone mass loss in the elderly population: Advances in diagnosis and treatment.” Journal of Biomedicine, Vol. 3 (2018): 40–49.
[2] Ji, M.-X., and Q. Yu. “Primary osteoporosis in postmenopausal women.” Chronic Diseases and Traslational Medicine, Vol. 1, No. 1 (2015): 9–13.
[3] Sen, R., and J. Hurley. “Osteoarthritis.” StatPearls[Internet], 2023-02-20, https://www.ncbi.nlm.nih.gov/books/NBK482326/.
[4] Padilla Colón et al. op. cit.
[5] Padilla Colón et al. op. cit.
[6] Porter, J.L., and M. Varacallo. “Osteoporosis.” StatPearls [Internet], 2022-09-04, https://www.ncbi.nlm.nih.gov/books/NBK441901/.
[7] Porter and Varacallo. op. cit.
[8] Porter and Varacallo. op. cit.
[9] Sen and Hurley. op. cit.
[10] Sen and Hurley. op. cit.
[11] Sen and Hurley. op. cit.
[12] Hong, A.R., and S.W. Kim. “Effects of resistance exercise on bone health.” Endocrinology and Metabolism, Vol. 33, No. 4 (2018): 435–444.
[13] Hong and Kim. op. cit.
[14] Muñoz-Garach, A., B. García-Fontana, and M. Muñoz-Torres. “Nutrients and dietary patterns related to osteoporosis.” Nutrients, Vol. 12, No. 7 (2020): 1986.
[15] Muñoz-Garach, García-Fontana, and Muñoz-Torres. op. cit.
[16] Eitner, A., and B. Wildemann. “Diabetes—osteoarthritis and joint pain.” Bone & Joint Research, Vol. 10, No. 5 (2021): 307–309.
[17] Eitner and Wildemann. op. cit.
[18] O’Keefe, J.H., N. Bergman, P. Carrera-Bastos, M. Fontes-Villalba, J.J. DiNicolantonio, and L. Cordain. “Nutritional strategies for skeletal and cardiovascular health: Hard bones, soft arteries, rather than vice versa.” Open Heart, Vol. 3, No. 1 (2016): e000325.
[19] O’Keefe et al. op. cit.
[20] Castelo-Branco, C., M.J. Cancelo Hidalgo, S. Palacios, M. Ciria-Recasens, A. Fernández-Pareja, C. Carbonell-Abella, J. Manasanch, and J. Haya-Palazuelos. “Efficacy and safety of ossein-hydroxyapatite complex versus calcium carbonate to prevent bone loss.” Climacteric, Vol. 23, No. 3 (2020): 252–258.
[21] Laird, E., M. Ward, E. McSorley, J.J. Strain, and J. Wallace. “Vitamin D and bone health: Potential mechanisms.” Nutrients, Vol. 2, No. 7 (2010): 693–724.
[22] Rodríguez-Olleros Rodríguez, C., and M. Díaz Curiel. “Vitamin K and bone health: A review on the effects of vitamin K deficiency and supplementation and the effect of non-vitamin K antagonist oral anticoagulants on different bone parameters.” Journal of Osteoporosis, Vol. 2019 (2019): 1–8.
[23] Rodríguez-Olleros Rodríguez and Díaz Curiel. op. cit.
[24] Bolland, M.J., A. Avenell, J.A. Baron, A. Grey, G.S. MacLennan, G.D. Gamble, and I.R. Reid. “Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: Meta-analysis.” BMJ, Vol. 341 (2010): c3691.
[25] Bolland et al. op. cit.
[26] Gregori, D., G. Giacovelli, C. Minto, B. Barbetta, F. Gualtieri, D. Azzolina, P. Vaghi, and L.C. Rovati. “Association of pharmacological treatments with long-term pain control in patients with knee osteoarthritis.” JAMA, Vol. 320, No. 24 (2018): 2564–2579.
[27] Richy, F., O. Bruyere, O. Ethgen, M. Cucherat, Y. Henrotin, and J.-Y. Reginster. “Structural and symptomatic efficacy of glucosamine and chondroitin in knee osteoarthritis: A comprehensive meta-analysis.” Archives of Internal Medicine, Vol. 163, No. 13 (2003): 1514–1522.
[28] Bucci, L.R., E. Sheldon, H. Schwartz, J. Pachon, D. Kalman, M. Mederos, J.C. Pezzullo, and C. Beer. “Comparison between glucosamine with chondroitin sulfate and glucosamine with chondroitin sulfate and hyaluronate for symptoms of knee osteoarthritis.” Osteoarthritis and Cartilage, Vol. 13, Supplement A (2005): P196, S99.
[29] Gregory et al. op. cit.
[30] Gregory et al. op. cit.
[31] Hume, A. “Glucosamine and chondroitin for osteoarthritis.” Pharmacy Today, Vol. 21, No. 11 (2015): 26.
[32] Hume. op. cit.

 Stores
Stores