Influencing the Gut Microbiota and Host Health: Naturopathic Perspectives
Would it surprise you to know that the human colon contains about 3.3 lb of bacteria?[1] This microbiota is practically its own organ, acting as an entire ecosystem with its own immune system, nervous system, and the ability to influence what the body absorbs from inside the intestinal lumen.
Consider the gut as the bridge between the inside of the body and the outside, connected by signals, nerves, compounds and other molecules. The gastrointestinal tract (GIT) is like a tube running from one end of your body to the other, acting as a barrier between what you ingest and what actually gets absorbed. Its job is to absorb nutrients and protect you from pathogens. However, at the same time, you have trillions of bacteria in there, working along this lining and determining influential aspects of your health.
The gut lining must stay tightly controlled to stop anything that you eat from just wandering into your bloodstream. These cells are susceptible to changes and inflammation, all related to what you’re eating (what the cells are exposed to) and the strains of bacteria species present.
Probiotic supplementation has been shown to reinforce the barrier of the intestinal lining.[2] This barrier not only decreases infections, but it also prevents reactions to food antigens, causing food sensitivities or IgG immune-system reactions. These reactions have been responsible for a multitude of symptoms such as gas, bloating, diarrhea, and eczema.
The composition of the gut microflora isn’t just based on probiotics supplementation, though. A poor diet can lead to a change in the species composition that colonizes the gut. The gut microbiota not only help to digest your leftovers from higher up in the intestines, but they actually produce their own cocktail of nutrients, neurotransmitter signals, and other chemicals that determine your health.
 The Role of the Gut Microbiota in Host Health
The Role of the Gut Microbiota in Host Health
The term “gut microbiota” is used to describe the multitude of species and colonies of bacteria and yeast in the GIT. The composition of the gut microbiota is influenced by diet, stress and environmental factors;[3] however, diet may play the largest role, attributing to 60% of the gut microflora.[1]
The diversity and density of gut microbiota is influenced by our diet, as bacteria feed on the undigested foods in the large intestine.[1] This includes resistant starches; nonstarch polysaccharides such as celluloses, pectins, and gums; as well as nondigestible oligosaccharides, often called “prebiotics.”[4]
This feeding drives the fermentation of carbohydrates in the colon and releases short-chain fatty acids for energy production for other, more specialized bacteria.[5] The metabolites produced by gut microbiota play crucial roles in host health. These metabolic products include regulators of cytokines, inflammation, and the immune system; visceral pain modulators via induction of opioid and cannabinoid receptors; and key nutrients such as folic acid and neurotransmitters such as GABA and serotonin.[1][6]
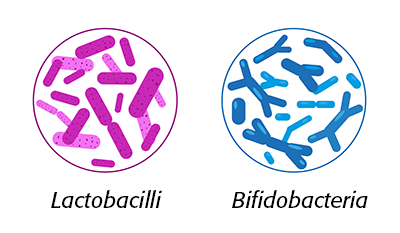
Lactic-acid bacteria are known to release various enzymes and vitamins, and have also been shown to affect the pH of the intestinal environment to inhibit the development of invasive pathogens such as Salmonella and E. coli strains.[2]
Any disturbance in this ecosystem by diet, pathogens, or antibiotics can lead to gut dysbiosis, and therefore, impaired activity of gut bacteria. This may result in negative effects on host health due to changes in intestinal-wall integrity and transit time of food through the GIT.[1][7] Additionally, gut dysbiosis has been associated with anxiety and depression, and animal studies have shown that probiotic supplementation may be a potential treatment for these mental-health conditions.[8]
 The Gut-Brain Connection
The Gut-Brain Connection
The gut-brain axis essentially is the connection between the enteric nervous system and the central nervous system (CNS), including all communications between the GIT and the brain. Gut bacteria play a critical role in the function of this axis as well as the hypothalamic-pituitary-adrenal axis and thus, stress-hormone release.[6][8]
Serotonin, a neurotransmitter, functions as a major signaling molecule in the enteric nervous system, functioning and overlapping with the CNS.[6] Tryptophan, a precursor to serotonin, is found in seeds, soybeans, meat, and fish. Tryptophan is absorbed in the gut and crosses the blood-brain barrier, where it is transformed into serotonin. Interestingly, the majority of serotonin in our bodies is actually located in the gut, synthesized by enterochromaffin (EC) cells. This production of serotonin is used to modulate the functioning of the GIT via secretion, peristalsis, vasodilation, and the perception of pain and nausea.[6]
Not only do EC cells synthesize serotonin, but gut bacteria also have the ability to produce serotonin from tryptophan and use it as a signal within the gut-brain axis to modify host behaviour.[6] Serotonin also helps to regulate the development of microvilli, the microscopic protrusions that increase the surface area of the intestinal lining to promote increased absorption of nutrients.[9]
Development and Maintenance of a Healthy Gut Microbiota
As mentioned above, diet plays a key role in the maintenance of beneficial gut microbiota. After all, these bacteria are feeding on the compounds and nutrients that are found in our GIT. Fibre plays an especially important role, and its absence can lead to bacterial migration. If their preferred food source isn’t available, bacteria will look to feed on other compounds, such as amino acids, releasing potentially harmful substances during metabolism.[5] These substances may contribute to inflammation and “leaky gut” issues, whereby intestinal permeability is altered and the tight junctions between intestinal cells lose their integrity. This process may influence the development of IBD or colon cancer, in addition to food sensitivities and/or allergies.[5]
Fermentation of dairy products, such as yogurt and kefir, with lactic-acid bacteria have multiple benefits on human health. Fermentation increases levels of vitamins B2 and B3 in yogurt.[2] One study of a yogurt produced with the species Lactobacillus bulgaricus showed that daily consumption significantly reduced the incidence of the common cold in elderly subjects.[10] These fermented dairy products may also help alleviate symptoms of lactose maldigestion.[10]
Current evidence is mounting that fermented foods may even help to promote cognitive health, enhance memory, and prevent neurotoxicity. Probiotic-rich diets have led to positive effects on stress relief, as gut bacteria are closely associated with hormonal stress responses.[8]
 Probiotics and Prebiotics
Probiotics and Prebiotics
Probiotics, by definition, are live microorganisms that are administered in high-enough doses to provide beneficial health outcomes to the host.[11] Probiotics can attenuate hormonal stress responses in addition to producing anxiolytic effects via GABA, glutamate, and serotonin production.[8][11] Abnormal stress responses have been observed in adults with gut dysbiosis, which can be reversed with proper colonization and restoration of the gut microbiota.[7] Probiotics and beneficial species of gut bacteria have been shown to support and modulate cortisol as well as reduce stress reactivity, and decrease social anxiety.[12]
Human studies are ongoing, some of which are investigating the involvement of gut microbiota in areas such as autism, Parkinson’s, and chronic pain. Strains most notable for their ability to improve anxiety, depression, and stress responses, in addition to gastrointestinal relief, include B. longum, B. breve, B. infantis, L. helveticus, L. rhamnosus, L. plantarum, and L. casei, with doses ranging from 10 million to 40 billion colony-forming units (CFU) per day.[11]
Prebiotics are typically nondigestible fibres that are used and/or consumed and fermented by bacteria of the microbiome. They have been shown to stimulate the growth and activity of beneficial microflora in the colon.[13] Often, there is a preference by Bifidobacteria to consume oligosaccharides, which can be found as a supplement or as part of a probiotic blend. Prebiotics also occur naturally in foods such as leeks, asparagus, chicory, Jerusalem artichokes, garlic, onions, and oats.[4]
Examples of functional fibres that induce health benefits to the host include inulin, beta-glucans, and xylooligosaccharides (XOS). These prebiotics each provide a unique carbon source for specific and selective support of different bacterial species. Therefore, the use of either one, individually, or in combination, can shape the population and colonization of specific bacterial species.
XOS is an emerging prebiotic naturally found in fruits, vegetables, milk, honey, and bamboo shoots. XOS, when given alone, has been shown to increase and benefit Bifidobacterium species within the gut microbiome. Most notably, XOS has been used clinically to improve the frequency of bowel movements and stool consistency.[13] XOS produces less gas than inulin, and therefore the tolerated dose of XOS is higher than inulin (found to be approximately 12 g/d).
Studies have shown that the introduction of XOS into the gut can significantly increase Bifidobacterium species within 24 hours. As well, there is a greater affinity of Bifidobacterium species to XOS than inulin or beta-glucans.[13]
 Conclusion
Conclusion
The colonization of the gastrointestinal tract by bacterial species influences several areas of our overall health, including digestion, mood and behaviour. The ability of the gut microflora to modulate cytokines and produce nutrients as well as neurotransmitters play key roles in signaling between the gut and other body systems such as the HPA axis, the immune system and the CNS. Their presence also protects us from infections by strengthening the barrier of intestinal cells separating the outside of the body (including what we ingest) from the inside of the body (within the bloodstream or body tissues).
Fermented foods, such as yogurt and kefir, in addition to prebiotic food ingredients, such as chicory and inulin, may serve as a vector for beneficial bacteria exposure. However, with equal importance is the maintenance of a high-fibre diet via vegetables, and grains such as oats, which feed these bacteria, allowing for the metabolic products which are so beneficial to our health.
References
- van Kylckama Klieg, J.E., et al. “Impact of microbial transformation of food on health—from fermented foods to fermentation in the gastro-intestinal tract.” Current Opinion in Biotechnology, Vol. 22, No. 2 (2011): 211–219.
- Parvez, S., et al. “Probiotics and their fermented food products are beneficial for health.” Journal of Applied Microbiology, Vol. 100, No. 6 (2006): 1171–1185.
- Lin, C.S., et al. “Impact of the gut microbiota, probiotics, and probiotics on human health and disease.” Biomedical Journal. Vol. 37, No. 5 (2014): 259–268.
- Savin, J. “Fiber and prebiotics: Mechanisms and health benefits.” Nutrients, Vol. 5, No. 4 (2013): 1417–1435.
- Marchesi, J.R., et al. “The gut microbiota and host health: A new clinical frontier.” Gut, Vol. 65, No. 2 (2016): 330–339.
- O’Mahony, S.M., et al. “Serotonin, tryptophan metabolism and the brain-gut–microbiome axis.” Behavioural Brain Research, Vol. 277 (2015): 32–48.
- Mayer, E.A., K. Tillisch, and A. Gupta. “Gut/brain axis and the microbiota.” The Journal of Clinical Investigation, Vol. 125, No. 3 (2015): 926–938.
- Kim, B., et al. “A review of fermented foods with beneficial effects on brain and cognitive function.” Preventive Nutrition and Food Science, Vol. 21, No. 4 (2016): 297–309.
- Nakamura, K., et al. “Role of a serotonin precursor in development of gut microvilli.” The American Journal of Pathology, Vol. 172, No. 2 (2008): 333–344.
- Morelli, L. “Yogurt, living cultures, and gut health.” The American Journal of Clinical Nutrition, Vol. 99, No. 5 Suppl. (2014): 1248S–1250S.
- Wang, H., et al. “Effect of probiotics on central nervous system functions in animals and humans: A systematic review.” Journal of Neurogastroenterology and Motility, Vol. 22, No. 4 (2016) 589–605.
- Misra, S., and D. Mohanty. “Psychobiotics: A new approach for treating mental illness?” Critical Reviews in Food Science and Nutrition, Vol. 59, No. 8 (2019): 1230–1236
- Carlson, J.L., et al. “Prebiotic dietary fiber and gut health: Comparing the in vitro fermentations of beta-glucan, inulin and xyloologsaccharide.” Nutrients, Vol. 9 No. 12 (2017): E1361.
Dr. Sarah Zadek, ND
A licensed naturopathic doctor in Ontario, who graduated from the Canadian College of Naturopathic Medicine in Toronto.
sarahzadeknd.com

 Stores
Stores